Trauma isn’t rare. According to the US Department of Veteran Affairs, 60 percent of men and 50 percent of women experience at least one trauma in their lives. Women are more likely to experience sexual assault and child sexual abuse. Men are more likely to experience accidents, physical assault, combat, disaster, or to witness death or injury. There is significant evidence supporting the correlation between trauma and developing substance use disorders. ACE Study author Dr. Vincent Felitti said:
“I would argue that the person using [drugs] is not using them to have a problem. They’re using drugs to find a solution.”
What is PTSD?
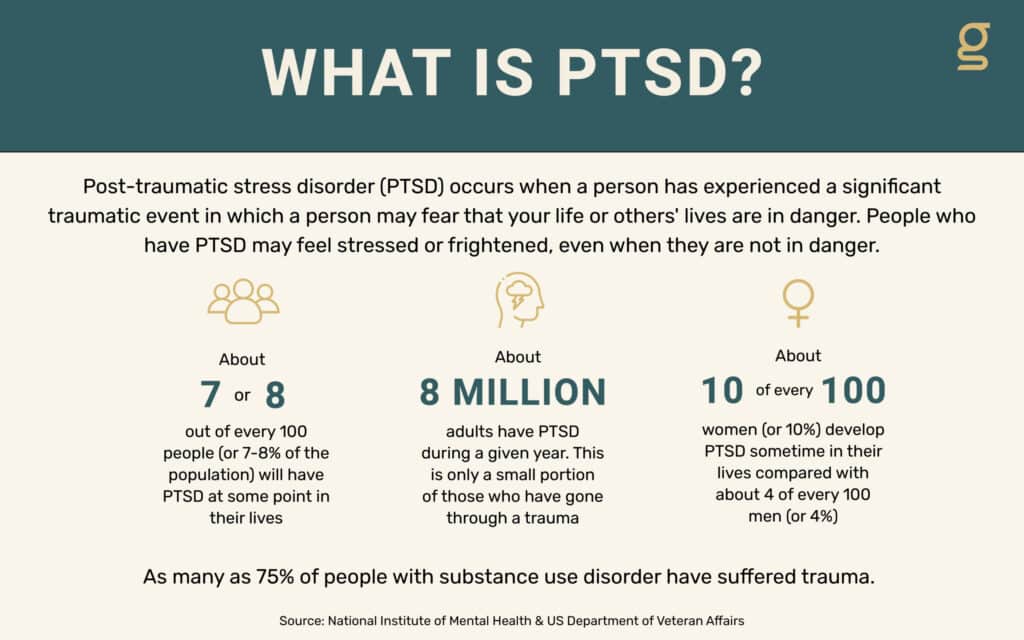
Post-traumatic stress disorder (PTSD) occurs when a person has experienced a significant traumatic event in which a person may fear that their life or others’ lives are in danger. People who have PTSD may feel stressed or frightened, even when they are not in danger.
Are you or someone you love struggling with PTSD? We are here to help.
Contact Us
Key Facts About PTSD
- About 7 or 8 out of every 100 people (or 7-8% of the population) will have PTSD at some point in their lives.
- About 8 million adults have PTSD during a given year. This is only a small portion of those who have gone through trauma.
- About 10 of every 100 women (or 10%) develop PTSD sometime in their lives, compared with about 4 of every 100 men (or 4%).
The Relationship Between PTSD and Addiction
As many as 75 percent of people with substance use disorder have suffered from trauma. We spoke to trauma expert and our clinical director, Steve Carleton, LCSW, CACIII, for an insight into this relationship.
In your experience, what is the prevalence of PTSD in those with substance use disorder?
After 14 years of treating addictions, my experience is that an overwhelming majority of those entering treatment have a history of trauma, adverse childhood experiences, or a significant loss or incident leading them to reach for a substance for relief. And the data supports this, reflecting that 75 percent of people struggling with addiction have experienced trauma or adverse experiences. Simply put, it is more the rule than the exception that someone struggling with addiction has experienced a trauma.
How might PTSD present in a person with SUD?
Great question! Unfortunately, it is not always obvious and doesn’t look the same for everyone. What is the same is what maintains symptoms of trauma – avoidance and stuck thinking. Avoidance is the most common and natural response when humans feel pain or discomfort. We are all programmed to resist threats, physical or emotional. With modern-day comforts, humans no longer have as many daily physical threats as compared to our ancestors, but we are still hard-wired to avoid in order to survive. Substance use, early on in its progression to addiction, can feel like a miracle to someone struggling with the effects of trauma. However, the incendiary nature of addiction leads to a vast array of consequences. Stuck thinking, on the other hand, prevents people from recovering from trauma. Our brain constantly makes efforts to protect us and give us a sense that we are in control. After a trauma, sometimes our brain will send us unhelpful messages to regain a sense of safety: “It was my fault” being at the top of this list. The majority of the time this is not so and causes problems downstream, but this, too, is hardwired in humans. The all too unfounded idea that “if it was my fault, then at least I can keep it from happening again.” It can feel unsafe for someone in the early days after a trauma to struggle with the idea that there might not have been anything different they could have done to prevent it.
How common is it for a person with SUD to be unaware that they have PTSD? What signs and symptoms should they be aware of?
With PTSD, memories of trauma feel intrusive and uncontrollable. The memories are persistent to the point that the body relives the experience. Again, there is an overwhelming urge to avoid people, places, things, objects that remind them of the trauma or cause that uncomfortable reaction. Shame-based thoughts that seek to blame or oversimplify the complex event. In addition to these, trouble concentrating, irritability and anger, anxiety, depression, trouble sleeping, constantly feeling on edge, strong persistent unwanted emotions, giving up activities, blocking details of the traumatic experience that don’t fit their beliefs, and difficulty connecting and letting people close to you. PTSD is more easily understood because it is usually a sudden and dramatic shift in mental health clearly resulting from a precipitating trauma.
What is the best way to approach trauma recovery with someone in early recovery?
I believe that as a community and society we all need to be more willing to listen and share stories about trauma and other painful experiences. We watch movies about fictitious characters experiencing harrowing events and at the same time never hear about traumas our friends or family members may have experienced. But to answer your question, let people know that you are willing to listen. Encourage them to share and confront painful memories and praise the hell out of them when they do. Let those tears/anger/confusion/whatever rip! Helpers do not have to have all the answers and do not have to have a Masters degree to be willing to listen.
There are some instances when sharing trauma can be dangerous or inappropriate but I encourage students and providers alike to ask about trauma. There is no evidence to suggest that a person sharing their trauma story, when they are ready (don’t push), will cause them long term harm. Quite the opposite when they find a provider or person willing to walk beside them.
As a clinician treating patients with SUD with trauma histories, how would you advise other clinicians to be more trauma-aware in their treatments?
It all starts with that first contact with a client. Most mental health providers can relate to the pressure felt in an initial assessment to ask pointed questions to gather the information we need to meet state and facility requirements. A pushy assessment is an invalidating experience for a client. More current modalities such as ACT approach assessment by gathering a client’s “life story” which gives the client more agency and autonomy to unpack their story how they choose. Motivational Interviewing (an EBP for addressing ambivalence to change) takes the stance that a formal assessment is a barrier to care. Anything we can do to make a client feel more comfortable and give them a sense of control in the treatment process goes a long way. Ask if they prefer to leave the door open when you meet, let them choose where to sit (if there are options), make sure they know they know they do not have to answer questions they don’t want to, learn and strive to accommodate preferences they might have for who and how treatment is provided, and don’t continue to pound away with questions when you start to sense that the client is withdrawing. Assessment should be an opportunity for the client to take a step back and reflect on their life experiences and connect the dots for themselves.
To learn more about complex trauma and how to effectively treat trauma, stay tuned for next week’s blog post. If we can help you or a person you love with their substance use disorder, please call today for a free and confidential assessment.


 Shannon Weir, RN
Shannon Weir, RN 
