Behind the Headlines
The headlines in 2024 seemed hopeful. Overdose deaths in America dropped by 27% compared to the previous year. Public health officials celebrated what the CDC called a major victory—more than 81 lives saved every day.
But a closer look at the data tells a more complicated story.
While overdoses declined in many parts of the country, they continued to rise dramatically in others. Some counties saw death rates jump by as much as 120% during the same period. And in Arizona, one of the states bucking the national trend, overdose deaths climbed back toward peak levels by early 2025.
Understanding why this is happening—and what it means for treatment—could save lives in communities that aren’t seeing the same progress as the rest of the nation.
The Numbers Tell Different Stories Depending on Where You Live
A recent investigation by The Guardian analyzed overdose data across all U.S. counties and found stark geographic disparities. The analysis, which examined data through December 2024, revealed that national averages can hide local crises.
The Guardian’s interactive data maps show the full picture: large swaths of the eastern United States saw significant decreases in overdose deaths, with some areas experiencing drops of 30% or more. But scattered across the map are clusters of brown and orange—counties where deaths increased, sometimes dramatically.
In Catoosa County, Georgia, overdoses increased by 120% since the national peak. Just a few hours away in Dougherty County, Georgia, deaths dropped by 74%. Georgia’s Department of Public Health admitted there’s “no clear cause” for this disparity in their own state.
Most notably for the southwestern United States, Arizona saw overdoses reach near-peak rates in early 2025. Delaware, Hawaii, Minnesota, New Mexico, and Washington also experienced increases after initially seeing declines.
Even as the national conversation celebrates progress, these communities are still in crisis.
Why Some Regions Still Struggle While Others Improve
Experts analyzing the data found that two factors emerged as the strongest predictors of whether overdoses were increasing or decreasing in a given area: changes in fentanyl prevalence and geography.
These two factors are connected. Research shows that fentanyl began replacing heroin in eastern states starting around 2013, then spread westward. The eastern United States experienced the worst of the fentanyl crisis earlier—and is now seeing more dramatic improvements. Western states are still in the thick of it.
Arizona’s Unique Challenges
Arizona faces specific obstacles that help explain why overdoses continue to climb there. According to a spokesperson for Arizona’s Medicaid office, the state’s proximity to major drug trafficking routes means the drug supply remains dangerous and unpredictable.
The situation is further complicated by polysubstance use. Arizona is increasingly seeing fentanyl combined with methamphetamine. This combination is more lethal than either drug alone and complicates medical response. When someone overdoses on multiple substances, standard interventions become less effective.
The Methamphetamine Factor
In several western states, including Washington, Oregon, and Arizona, methamphetamine appears closely tied to overdose rates. This matters because most overdose prevention resources focus on opioids. Naloxone, for example, only reverses opioid overdoses—it does nothing for stimulant overdoses.
People struggling with methamphetamine use often have trouble finding appropriate treatment because funding and programs remain heavily focused on opioid-related interventions.
Naloxone Saves Lives, But It’s Not Enough
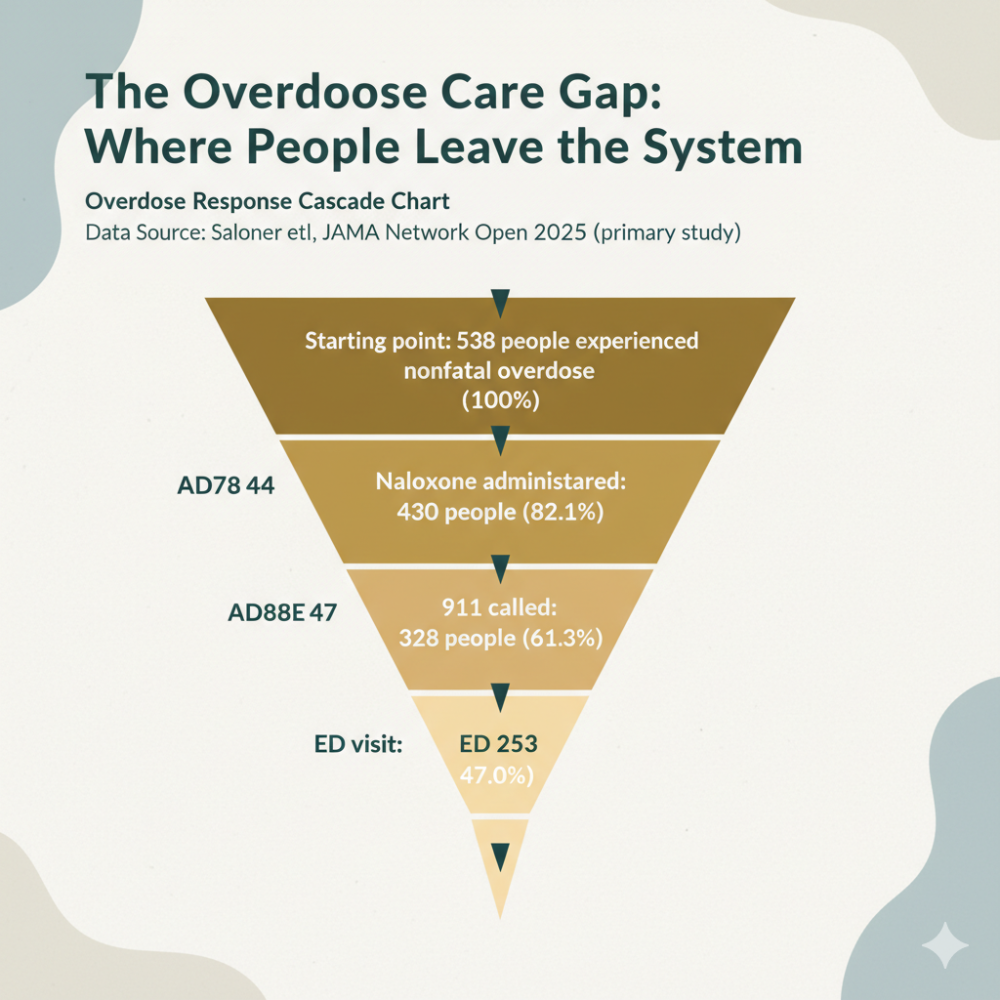
Nearly every discussion about declining overdose deaths mentions naloxone first. The overdose-reversal medication is widely available now—you can get it at most pharmacies without a prescription, and many community organizations distribute it for free.
Naloxone absolutely saves lives. Every expert agrees on this.
But here’s what often gets lost in the celebration: naloxone is an emergency intervention, not a solution. Dr. Marc Fishman, an addiction psychiatrist at Johns Hopkins University, put it bluntly: “You can’t say I’m gonna reverse an acute overdose and then celebrate when you haven’t addressed the disorder.”
Every time someone needs naloxone, they were already on the edge of death. Without it, they would likely have died. With it, they wake up in immediate withdrawal. What happens next determines whether they survive long-term.
The Real Question: What Happens After the Naloxone?
Public health experts emphasize that preventing overdose deaths requires more than keeping naloxone handy. It requires addressing addiction itself through sustained treatment and mental health care.
Andrew Kolodny, medical director for the opioid policy research collaborative at Brandeis University, used a powerful analogy: During the AIDS crisis, thousands died from PCP pneumonia. But we didn’t call it a “PCP pneumonia epidemic.” We recognized that HIV was the underlying disease, and we addressed it with prevention and treatment.
“This is a crisis of addiction,” Kolodny explained. “Most of these deaths are occurring in people who are addicted, not people saying, ‘Hey, shooting up fentanyl would be a fun way to spend a Friday night.’ It’s people who are really struggling.”
Why We’re Flying Blind in Some Communities
One of the most concerning findings from The Guardian’s investigation isn’t about overdoses themselves—it’s about how little real-time information many communities have about what’s happening.
In most of the country, officials may never know the underlying cause of a local spike in overdoses. Data on drug composition and toxicology can take months to become available, if it becomes available at all.
Some places are doing better. In Cook County, Illinois (which includes Chicago), toxicology reports can be available in less than a month. Chicago tracks the drug supply, ambulance data, and other information to pinpoint overdose spikes at the neighborhood level and respond quickly.
But Chicago is the exception. Most communities lack the resources, coordination, or data to respond effectively to local changes in the drug supply.
What’s Actually in the Drug Supply?
The Drug Enforcement Administration announced that fentanyl purity has been decreasing recently. This likely explains some of the decline in overdoses. When fentanyl became more expensive for cartels to manufacture, less of it entered the United States.
But the DEA won’t share regionally specific data on drug purity—not with the public, and not even with public health researchers trying to save lives.
Without this information, local health departments can’t allocate resources effectively. They can’t know whether to focus on opioids, stimulants, or combinations of drugs. They’re essentially guessing about how to protect their communities.
What Actually Works: Medical Treatment and Long-Term Support
The data makes one thing clear: emergency response alone won’t solve the overdose crisis. Communities need robust treatment infrastructure.
Medical detoxification is often the first crucial step for people with substance use disorders. Withdrawal from opioids, especially high-dose fentanyl, is physically and psychologically brutal. Withdrawal from benzodiazepines or alcohol can be life-threatening. Complex cases involving multiple substances require specialized medical expertise.
During medical detox, healthcare professionals can:
– Monitor vital signs and adjust medications in real-time
– Address co-occurring medical conditions
– Begin treatment for mental health conditions often underlying addiction
– Create a safe, supportive environment during the most vulnerable period
– Connect individuals to ongoing treatment and support
After detox, intensive outpatient programs, counseling, peer support, and sometimes medication-assisted treatment help people build lives in recovery. This is where lasting change happens.
Regional Solutions for Regional Problems
The geographic disparities in overdose trends mean that national statistics can be misleading. What works in Philadelphia might not work in Phoenix. What’s needed in Seattle might be different from what’s needed in Atlanta.
Arizona’s challenges with border proximity, polysubstance use, and continuing fentanyl prevalence require tailored responses. Western states with high methamphetamine use need different resources than eastern states primarily dealing with opioids.
Local treatment providers who understand their community’s specific drug supply and population needs are essential. Facilities that can handle complex medical cases, multiple substance dependencies, and co-occurring conditions play a vital role in regions where the crisis continues to worsen.
Finding Hope in the Data
Despite the concerning regional increases, there are reasons for optimism buried in the numbers.
First, many communities have proven that overdose deaths can decline dramatically. The fact that some areas saw 30-40% reductions shows that progress is possible. These success stories offer blueprints for struggling communities.
Second, experts now better understand the factors driving regional differences. This knowledge can inform more targeted interventions.
Third, awareness is growing that addiction treatment—not just overdose prevention—must be the priority. As Dr. Fishman noted, if the trend continues downward, moving from 80,000 deaths to 70,000 to 60,000, that would be real progress worth celebrating.
What This Means for Individuals and Families
If you or someone you love is struggling with substance use, these statistics represent something more than data points. They represent the reality that geography shouldn’t determine whether you survive.
The complex nature of today’s drug supply—with powerful synthetic opioids, stimulants, and unpredictable combinations—makes professional medical treatment more important than ever. Self-detox or “cold turkey” approaches are not only dangerous, they’re increasingly ineffective for the substances people are using today.
Seeking treatment is an act of courage. Finding a facility equipped to handle complex cases, provide 24/7 medical supervision, and create individualized protocols can mean the difference between successful recovery and another statistic.
Moving Forward: Treatment as Prevention
The Guardian’s analysis reveals an uncomfortable truth: we’ve been focused on measuring deaths while under-investing in preventing addiction and treating the underlying disorder.
Better data helps, but data alone doesn’t save lives. Treatment does. Medical care does. Long-term support does.
The regions seeing continued increases in overdose deaths need more than naloxone distribution. They need expanded access to medical detox, intensive outpatient programs, mental health services, and sustained recovery support.
For individuals caught in the cycle of substance use, particularly in regions where the crisis is worsening, knowing that professional help exists matters. The most effective programs combine immediate medical stabilization with evidence-based long-term treatment.
Overdose deaths may be declining nationally, but if your community is among those still seeing increases, that national statistic offers little comfort. What matters is access to comprehensive, medically supervised treatment where you live.
The data shows that when people receive appropriate care at the right level of intensity, recovery is possible. Behind every percentage point in these analyses are real people—and many of them are getting the help they need and building lives in recovery.
—
References and Sources
Hannah Harris Green and Matt Kiefer. “Overdose in America: analysis reveals deaths rising in some regions even as US sees national decline.” *The Guardian, October 17, 2025. https://www.theguardian.com/us-news/ng-interactive/2025/oct/17/overdose-deaths-data-analysis
*Primary source for this article; includes interactive maps showing county-level overdose trends across the United States from August 2023 to December 2024. The investigation analyzed CDC mortality data, Census Bureau demographics, drug seizure data, and urine analysis results to identify geographic patterns in the overdose crisis.*
Centers for Disease Control and Prevention. “Drug Overdose Deaths in the U.S. Top 106,000 in 2021.” CDC Press Release, May 2022.
*Official CDC data on overdose mortality trends. The CDC reported a 27% decline in overdose deaths in 2024, translating to approximately 81 lives saved daily, though 220 Americans still died of overdose each day on average.*
Centers for Disease Control and Prevention. “Understanding the Opioid Overdose Epidemic.” CDC Injury Prevention & Control, 2025.
*Comprehensive CDC resource explaining the three waves of the opioid epidemic, the role of synthetic opioids like fentanyl, and evidence-based prevention strategies including naloxone distribution and medication-assisted treatment.*
Substance Abuse and Mental Health Services Administration (SAMHSA). “National Survey on Drug Use and Health (NSDUH).” 2024.
*Federal survey providing national and state-level estimates of substance use and mental health conditions. Experts quoted in The Guardian article noted limitations in this data collection approach for tracking addiction trends accurately at the community level.*
Friedman J, Mann NC, Hansen H, et al. “Increasing fentanyl-related overdose deaths across the USA.” *The Lancet*, September 2021.
*Peer-reviewed research documenting the geographic spread of fentanyl across the United States, beginning in eastern states around 2013 and moving westward, driving profound increases in overdose mortality.*
Drug Enforcement Administration. “2024 National Drug Threat Assessment.” U.S. Department of Justice, 2024.
*Federal assessment of drug trafficking and supply trends. The DEA reported decreasing fentanyl purity in recent assessments, though the agency does not share regionally specific purity data with public health researchers.*
Arizona Health Care Cost Containment System (AHCCCS). Statement on rising overdose deaths in Arizona, 2025.
*State Medicaid office statement identifying synthetic opioids (especially fentanyl) combined with stimulants like methamphetamine as primary drivers of Arizona’s rising overdose rates, and noting the state’s unique challenges due to proximity to major drug trafficking routes.*
Georgia Department of Public Health. Statement on county-level overdose disparities, 2025.
*State health department acknowledgment of significant variations in overdose trends across Georgia counties, emphasizing the need for better surveillance and data-sharing to help local partners focus efforts on specific populations and risk factors.*
Institute for Health Metrics and Evaluation (IHME).”Opioid Use Disorder.” Global Health Data Exchange, 2024.
*Global health research data comparing international responses to opioid crises. Portugal’s approach, which includes comprehensive addiction tracking and multi-agency coordination, has resulted in a per capita overdose death rate less than 1/30th that of the United States.*
National Institute on Drug Abuse (NIDA). “Naloxone for Opioid Overdose: Life-Saving Science.” National Institutes of Health, 2024.
*Federal research institute’s explanation of how naloxone works to reverse opioid overdoses by blocking opioid receptors in the brain, and evidence supporting its effectiveness in emergency overdose response.*
American Society of Addiction Medicine (ASAM). “The ASAM Criteria: Treatment Criteria for Addictive, Substance-Related, and Co-Occurring Conditions.” 4th Edition, 2024.
*Professional clinical guidelines for matching individuals with substance use disorders to appropriate levels of care, from outpatient counseling through medically monitored intensive inpatient treatment (Level III.7-D), based on severity and complexity of needs.*