Why Half of Overdose Survivors Never Reach the Hospital: Understanding the Gap in Emergency Care
Introduction
When someone survives a drug overdose, getting to a hospital might seem like the obvious next step. But new research published in JAMA Network Open reveals a troubling reality: fewer than half of people who experience a nonfatal overdose ever make it to an emergency department for medical care.
This gap represents both a challenge and an opportunity. While it’s encouraging that naloxone is saving lives in the community, the lack of follow-up medical care means many people miss critical chances to access treatment, medications, and resources that could prevent future overdoses.
Understanding why people avoid emergency care after an overdose—and what can be done about it—is essential for anyone concerned about the overdose crisis affecting communities nationwide.
The Research: A Closer Look at Overdose Response
What the Study Found
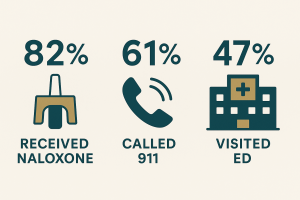
Researchers surveyed over 2,000 adults who had used opioids, cocaine, or methamphetamines in the previous year across Wisconsin, Michigan, New Jersey, and New Mexico. Among those who had experienced at least one nonfatal overdose:
- 82% had naloxone administered during their most recent overdose
- 61% had someone call 911 for emergency help
- Only 47% actually visited an emergency department for medical evaluation
These numbers tell an important story. Naloxone—the life-saving medication that reverses opioid overdoses—is reaching people and working as intended. But the connection to formal medical care is breaking down somewhere along the way.
Who’s Most Likely to Seek Care
The study identified some patterns in who does and doesn’t receive emergency medical care:
People were more likely to have 911 called if they:
- Were Black compared to White individuals
- Lived in New Jersey compared to Wisconsin
- Used drugs occasionally rather than daily or not at all
Interestingly, researchers found that having Medicaid insurance was associated with higher rates of naloxone use, suggesting that access to harm reduction services matters.
Why People Don’t Call 911 After an Overdose
Understanding the reasons behind avoiding emergency care helps us address the problem more effectively.
Managing Without Medical Help
The most common reason people gave for not calling 911 was simple: they felt they didn’t need it.
Nearly 29% of respondents said the person regained consciousness without naloxone. Another 27% reported that a bystander successfully administered naloxone and the person recovered. In these situations, people made a judgment call that medical intervention wasn’t necessary.
This reflects a complex reality. While medical evaluation after any overdose is strongly recommended, people who use drugs often develop their own safety protocols and may feel confident managing certain situations without formal medical help.
Fear of Law Enforcement
Fear of police involvement was the third most common reason for not calling 911, cited by about 22% of respondents who didn’t seek emergency help.
This fear isn’t unfounded. Despite Good Samaritan laws in many states that provide some legal protection for people who call for help during an overdose, concerns about arrest, harassment, or other consequences remain significant barriers. People may worry about:
- Outstanding warrants or probation violations
- Drug possession charges
- Child protective services involvement
- Housing consequences
- Immigration status issues
Past Negative Experiences
Previous interactions with emergency medical services and hospitals can strongly influence whether someone seeks care after an overdose. People with substance use disorders frequently report experiencing:
- Stigma and judgmental treatment from medical staff
- Inadequate pain management during withdrawal
- Feeling pressured or coerced into treatment
- Long wait times with minimal support
- Discharge without connection to ongoing care
When someone has faced these challenges before, they may reasonably conclude that going to the hospital won’t help—or might even make things worse.
What Happens When People Do Go to the Hospital
For those who made it to an emergency department, the study found mixed results in terms of the care they received.
The Good News
Most people who visited the ED received some form of support:
- 62% received take-home naloxone to prevent future fatal overdoses
- 52% got an appointment for drug treatment services
- 34% received care for non-overdose health concerns
Having naloxone available when leaving the hospital is crucial. People who have experienced one overdose are at significantly higher risk of having another, especially in the days immediately following the first event.
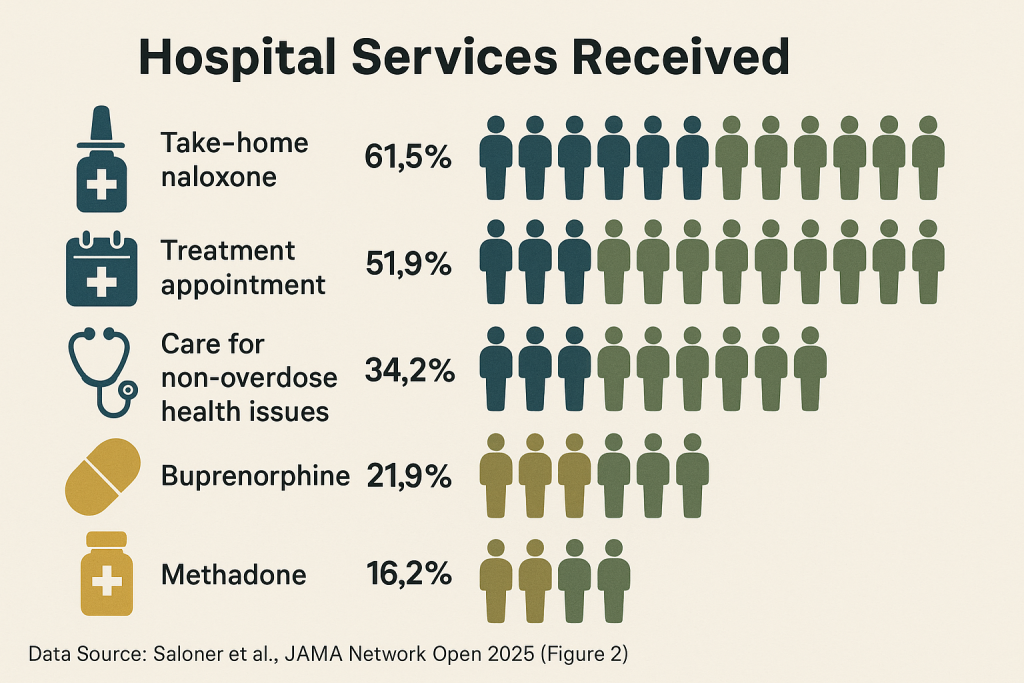
The Gap in Medication Treatment
The study revealed a concerning gap: only about one in five people (22%) received buprenorphine before leaving the hospital, and just 16% received methadone.
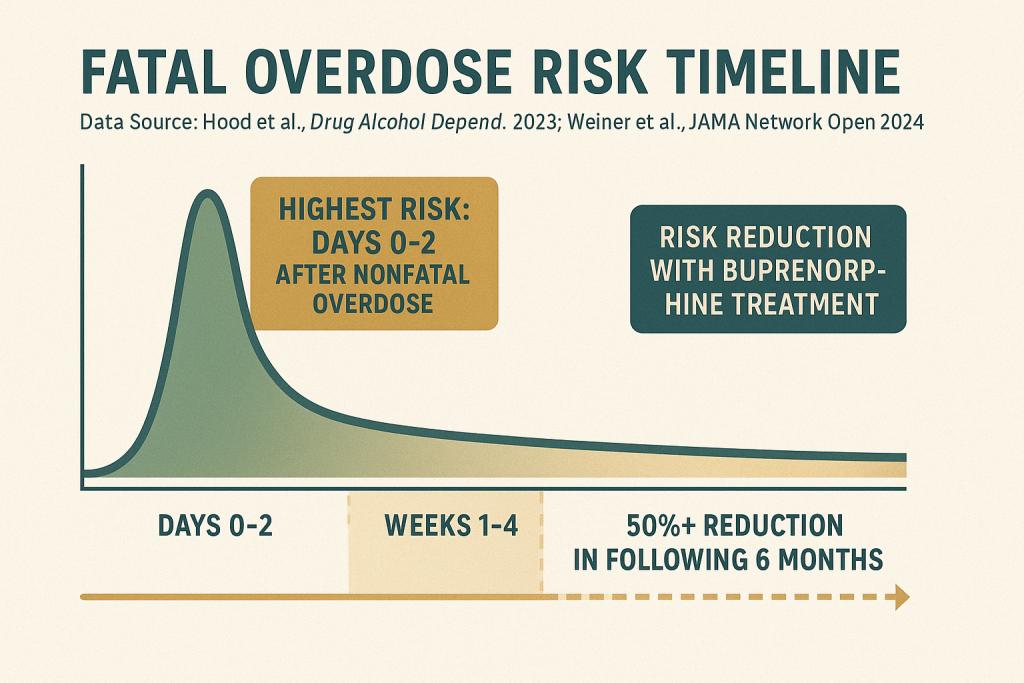
This matters enormously. Research consistently shows that medications for opioid use disorder—particularly buprenorphine—substantially reduce overdose risk in the weeks and months following an overdose. Starting these medications in the hospital has been linked to better long-term outcomes and increased engagement with continuing care.
The low rates of medication initiation represent a significant missed opportunity to provide evidence-based treatment at a critical moment.
The Critical Importance of Medical Evaluation After Overdose
Why Emergency Care Matters
Even when someone appears to have fully recovered from an overdose, medical evaluation serves several vital purposes:
Assessing for complications: Overdoses can cause injuries or medical problems that aren’t immediately obvious. These might include aspiration pneumonia, rhabdomyolysis (muscle breakdown), or cardiac issues.
Monitoring for delayed effects: Some substances, particularly long-acting opioids or combinations of drugs, can cause delayed or recurring symptoms that require extended observation.
Preventing immediate re-overdose: The period immediately after an overdose is extremely high-risk. Having medical supervision and appropriate medications can prevent another overdose in the critical hours and days that follow.
Connecting to treatment: For many people, surviving an overdose creates a window of opportunity—a moment when they may be more open to considering treatment options. Emergency departments can serve as a bridge to longer-term care.
The Two-Day Window
Research has shown that people face the highest risk of fatal overdose in the two days immediately following a nonfatal overdose. This makes prompt medical intervention and connection to ongoing care absolutely critical.
How Medical Detox Can Help
When Hospitalization Isn’t Enough
While emergency departments provide essential acute care, they’re not designed for the comprehensive medical management that many people need after an overdose—especially if they’re experiencing withdrawal or have been using substances regularly.
This is where specialized medical detoxification becomes important.
The Role of Medical Detox Facilities
Medical detox programs like those offered at Gallus Detox provide:
24/7 medical supervision by physicians and nurses specially trained in addiction medicine and withdrawal management
Individualized medication protocols that address both safety and comfort during the withdrawal process
Treatment for co-occurring medical conditions that may have been identified or worsened by the overdose
A safe, supportive environment without stigma or judgment
Connection to continuing care including intensive outpatient programs and long-term treatment planning
The Gallus Approach After Overdose
For someone who has experienced an overdose, specialized medical detox offers several advantages:
Proper assessment: Comprehensive medical evaluation to identify any complications from the overdose and develop a complete treatment plan.
Comfort during withdrawal: The Gallus Method uses proprietary combinations of IV and oral medications to minimize withdrawal symptoms and support the body’s natural healing processes.
Medication initiation: Starting medications for opioid use disorder (when appropriate) in a medically supervised setting with proper dosing and monitoring.
Treatment planning: Working with the person to understand their goals and develop a realistic, individualized plan for ongoing recovery support.
Alternative Pathways to Care
Not everyone who survives an overdose without going to the hospital is ready for residential detox or formal treatment. That’s okay. Recovery looks different for everyone, and there are multiple ways to increase safety and access support.
Harm Reduction Services
Harm reduction programs provide vital support without requiring abstinence or formal treatment enrollment:
- Regular access to naloxone and overdose prevention education
- Fentanyl test strips to check drugs for dangerous contaminants
- Connection to peer support specialists with lived experience
Intensive Outpatient Programs
For people who want support but need to maintain work or family commitments, intensive outpatient programs (IOP) offer:
- Regular group and individual counseling
- Skills development for managing triggers and preventing relapse
- Both in-person and virtual options
Gallus Outpatient Services provides these programs for people at various stages of recovery, whether they’re transitioning from detox or seeking support while managing their substance use in the community.
Peer Recovery Support
Sometimes the most powerful intervention comes from someone who has been through similar experiences. Peer recovery specialists can:
- Meet people where they are without judgment
- Share their own experiences and what helped them
- Help navigate the healthcare system and connect to resources
- Provide ongoing support and encouragement
The Path Forward: Bridging the Gap
The finding that fewer than half of overdose survivors receive emergency medical care reveals both challenges and opportunities.
What Needs to Change
Expanding community-based interventions: Since many people manage overdoses without formal medical systems, we need to ensure community responders have the training, medications, and connections to care they need.
Reducing criminalization: Fear of law enforcement remains a significant barrier. Policies that truly protect people who seek help during overdoses can save lives.
Improving hospital care quality: When people do go to the hospital, they should receive evidence-based treatment including medications for opioid use disorder and warm connections to ongoing care.
Hope in the Numbers
Despite the concerning gaps, there are encouraging signs in this research:
The widespread availability of naloxone in the community is working. More than 80% of overdose survivors had naloxone administered, showing that harm reduction efforts are reaching people who need them.
When people do access emergency care, they often receive important resources like naloxone and treatment referrals.
Communities are increasingly recognizing that traditional emergency response models don’t serve everyone, leading to innovation in alternative approaches.
Conclusion: Every Overdose Survivor Deserves Support
Surviving an overdose is both a crisis and an opportunity—a moment when the right support and resources can change the trajectory of someone’s life.
Whether that support comes through a 911 call and emergency department visit, a peer specialist with naloxone, a harm reduction program, or a medical detox facility, what matters most is that it’s available, accessible, and delivered without judgment.
If you or someone you care about has experienced an overdose, please know: help is available, recovery is possible, and you deserve compassionate, expert care.
Medical detoxification at a specialized facility like Gallus Detox can provide the comprehensive medical support, comfortable withdrawal management, and connection to ongoing care that helps people move forward after an overdose. Our team understands the complexity of these situations and is here to help 24 hours a day, 7 days a week.
If you’re ready to talk about treatment options, call Gallus Detox at 844-800-3607. Admissions specialists are available to answer questions and begin the admission process.
You may also contact SAMHSA about other options for help:
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you.
The Substance Abuse and Mental Health Services Administration (SAMHSA) is the agency within the U.S. Department of Health and Human Services that leads public health efforts to advance the behavioral health of the nation.
Idea for researching this blog post came via an article from medical express (Fewer than half of drug overdose survivors go to the hospital – by Lori Solomon, edited by Gaby Clark, reviewed by Alexander Pol Oct 2025 – https://medicalxpress.com/news/2025-10-drug-overdose-survivors-hospital.html ) popping into our personalized news feed.
Additional research sources:
Annotated References
- Saloner B, Fredericks PJ, Byrne L, et al. Naloxone Use, 911 Calls, and Emergency Visits After Nonfatal Overdose. JAMA Network Open. 2025;8(10):e2537678.
- Primary source for this article. Multistate survey of 2,097 people who use drugs examining service engagement after nonfatal overdose. Provides data on rates of naloxone use, 911 calls, and ED visits, as well as reasons for not seeking care.
- Weiner SG, Little K, Yoo J, et al. Opioid Overdose After Medication for Opioid Use Disorder Initiation Following Hospitalization or ED Visit. JAMA Network Open. 2024;7(7):e2423954.
- Research demonstrating that buprenorphine use immediately following hospitalization substantially reduces overdose risk in the following six months. Supports recommendations for ED-initiated medications for opioid use disorder.
- Hood JE, Aleshin-Guendel S, Poel A, et al. Overdose and Mortality Risk Following a Non-Fatal Opioid Overdose Treated by Emergency Medical Services in King County, Washington. Drug Alcohol Depend. 2023;253:111009.
- Study showing elevated risk of fatal overdose following nonfatal overdose, particularly in the first two days. Demonstrates the critical importance of post-overdose interventions.
- Herring AA, Rosen AD, Samuels EA, et al. Emergency Department Access to Buprenorphine for Opioid Use Disorder. JAMA Network Open. 2024;7(1):e2353771.
- Research on emergency department buprenorphine initiation and its association with increased engagement in ongoing treatment. Supports hospital-based medication initiation protocols.
- Hawk K, Grau LE, Fiellin DA, et al. A Qualitative Study of Emergency Department Patients Who Survived an Opioid Overdose: Perspectives on Treatment and Unmet Needs. Academic Emergency Medicine. 2021;28(5):542-552.
- Qualitative research exploring the perspectives of overdose survivors regarding treatment and barriers to care. Provides insight into patient experiences with emergency care.
- Richardson NJ, Ray B, Smiley-McDonald HM, Davis CS, Kral AH. National Survey Findings on Law Enforcement Agency Drug Response Practices, Overdose Victim Outcomes, and Good Samaritan Laws. Drug Alcohol Depend. 2023;248:109916.
- Study examining the impact of Good Samaritan laws and law enforcement practices on overdose response. Relevant to understanding fear of criminalization as a barrier to seeking help.
- Carroll G, Solomon KT, Heil J, et al. Impact of Administering Buprenorphine to Overdose Survivors Using Emergency Medical Services. Annals of Emergency Medicine. 2023;81(2):165-175.
- Research on prehospital buprenorphine programs showing improved outcomes for both patients who decline transport and those who receive further ED care.
- Centers for Disease Control and Prevention. Drug Overdose Deaths in the United States, 2003–2023. NCHS Data Brief No. 522. December 2024.
- Government data on overdose mortality trends providing context for the current state of the overdose crisis and recent declines in some areas.
- National EMS Information System (NEMSIS). Drug Overdose Surveillance Dashboard. August 2025.
- Federal data on EMS encounters for nonfatal overdoses, showing approximately 650,000 encounters in 12 months with 17% not transported by medical personnel.
- Vadiei N, Axon DR, Eckert B. Naloxone Distribution Models in the United States: A Scoping Review. Substance Use & Addiction Journal. 2025;46(2):391-404.
- Review of naloxone distribution programs including pharmacies, community programs, and over-the-counter access. Provides context for widespread naloxone availability mentioned in study.



